NEUROSURGERY is a highly specialized surgical subspecialty that involves i) medical treatments ii) physical treatments iii) interventional or endovascular procedures and iv) minimally invasive microsurgeries for treating a very wide spectrum of clinical conditions and diseases that happen at our BRAIN and SPINE. Among all, treating STROKE and PAIN are the basics of Neurosurgery daily practices.
In the other words, NEUROSURGEONs, with their knowledges and trainings, together with their sophisticated micro-instruments, utilize their operative skills under the microscope, they treat wide spectrum of clinical conditions and diseases that happen along human nervous systems and its surrounding tissues; skull, spinal column, vessels and related tissues.
The followings are the summary of the common routines in Neurosurgical Practices:
with numbness, pain, weakness at arms or legs, sciatica pain at legs.
with spinal cord or cauda equina nerves compressions, causing pain, numbness, weakness at arms or legs, disturbed gait, disturbed urinary habit and bowel habits, disturbed sexual function.
with back pain, nerves compressions, spinal instability or scoliosis:
Minimally Invasive Spine Fusion Surgery under Microscope:Among all Neurosurgeries, minimally invasive spine surgery (MIS Spine Surgery) are the microsurgeries that Neurosurgeons most commonly perform among their routines.
For all spine surgeries, Neurosurgeons apply their knowledges of nervous system and spinal column, and also their microsurgical skills and techniques, together with their micro-instruments of brain surgeries. Sometimes, Neurosurgeons may also add the technique of Continuous Intra-Operative Neural Monitoring (IOM) to monitor the nerve signal transmission function along brain, spinal cord and nerves during surgery, so as to assure patients’ good neurological outcome in spine surgeries.
With the ever-advancing Medical Technology, seeking a second medical opinion is now the standard practice for all kinds of medical diagnoses. Getting a second medical opinion from another Medical Expert is a decision-support tool for ratification or modification of the medical suggestions from other doctors.
Second medical opinion may have critical impacts on the disease outcome by influencing the followings, namely 5Cs:
Brain tumors can be subdivided into non-cancerous benign tumor and malignant cancerous tumor. If a tumor is originated within brain compartment ......
Tumors can develop in the vertebrae, nerves, and other tissue throughout your spine. Some spine tumors, such as astrocytomas, occur more commonly in children and adolescents......
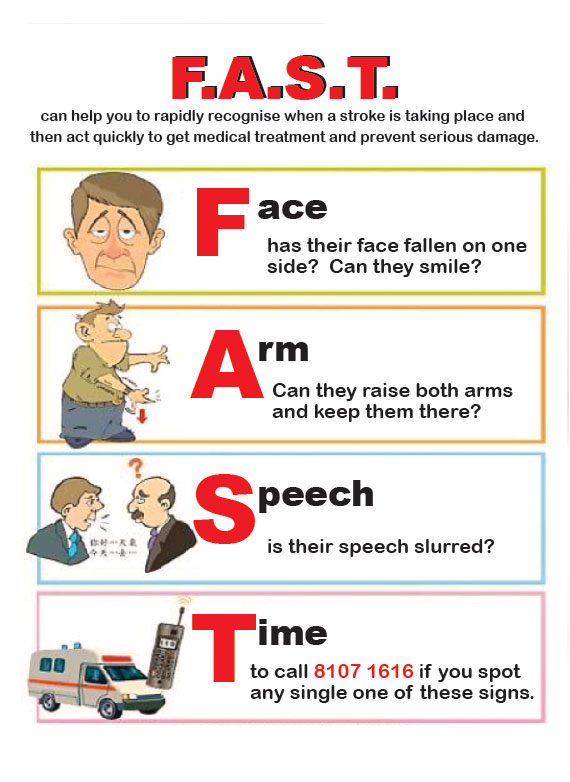
Given the disease burden of strokes, prevention is an important public health concern. As stroke neurosurgeons, we do not want to treat stroke unless we are forced to do so for acute stroke ......
Brain tumors grow and compress normal brain tissue. Both benign and malignant tumors can cause swelling of the brain and raised intracranial pressure. Headache, dizziness....
Given the disease burden of strokes, prevention is an important public health concern. As stroke neurosurgeons, we do not want to treat stroke unless we are forced to do so for acute stroke treatments in emergency setting; we actually want to prevent stroke by promoting stroke risks screening program & stroke prophylactic treatments. 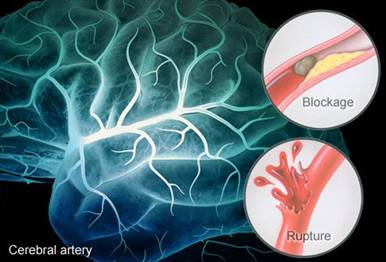
Is stroke survivor prone to more strokes in future life?
Yes— The risk of stroke for someone who has already had one is many times that of a person who has not. If you've had a heart attack, you're also at higher risk of having a stroke, too.
Search and Treat the Real Cause of Stroke to Prevent Further Stroke within short period of time:
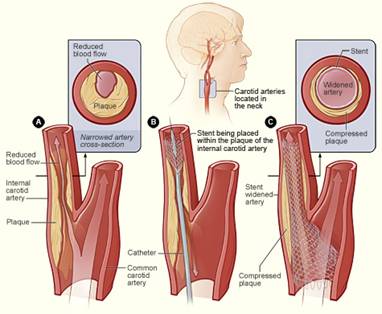
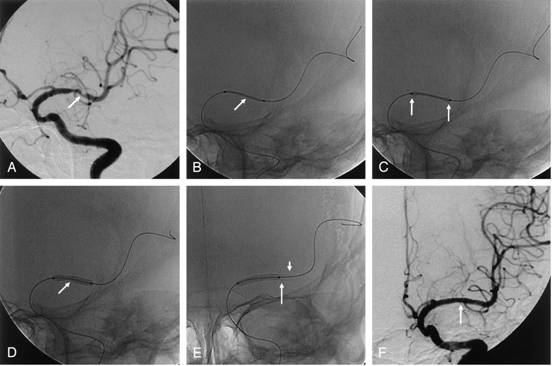
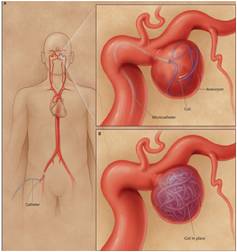
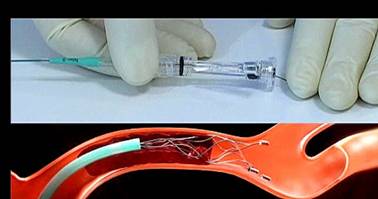
With traditional stroke treatments, most treatments were just empirical medications, without searching for the real cause of stroke; nowadays Stroke Neurosurgeons prefer high quality MRI angiogram or cerebral angiogram to search for the real cause of stroke and treat accordingly; so as to prevent stroke from recurring within short period of time.
Stroke prophylactic treatments





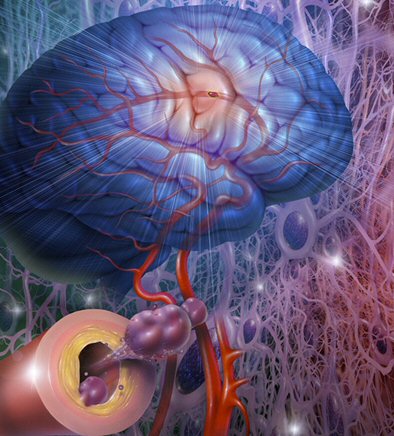
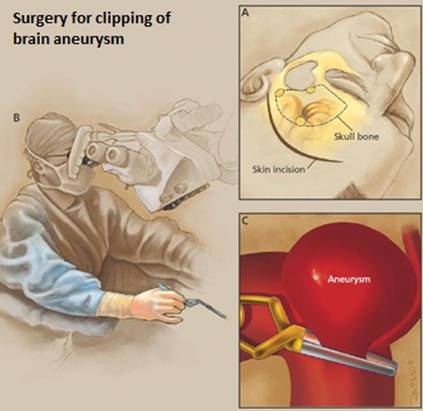


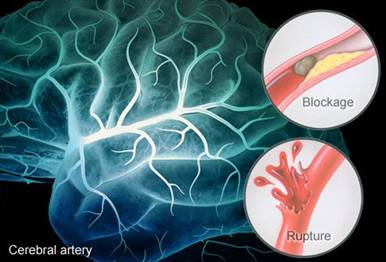
 Stroke is formed as a result of cerebral vascular deficits, its incidence increases exponentially from 30 years of age. In fact, the signs of stroke are traceable through risk screening, in which we can identify the health status of the cerebral vessels, intervention can be taken to lower the risk of strokes.
Stroke is formed as a result of cerebral vascular deficits, its incidence increases exponentially from 30 years of age. In fact, the signs of stroke are traceable through risk screening, in which we can identify the health status of the cerebral vessels, intervention can be taken to lower the risk of strokes.
It is advised to conduct a regular brain check up, and the frequency depends on your age group as follow:
| Age | Frequency | ||
| 30-40 years old | 5 - 8 years | ||
| 40-60 years old | 5 years | ||
| over 60 years old | 3 - 5 years |
HKBSSP offers a comprehensive Stroke Screening Programme, screening individuals for known risk factors of stroke and implementing management of modifiable risk factors, the programme includes:
Our vascular neurosurgeon will evaluate the test results from the above items, and will recommend further neuro-radiological imaging, electro-neuro-physiological study & any related tests if necessary.
For further information of what each item includes and price, please contact us via +852 2367 6116 or make booking now.
Since both stroke and heart attack are caused by vascular diseases of various causes. Modern medicine and Stroke Neurosurgeon nowadays consider stroke as ‘brain attack’ its care, either preventive or emergency treatments are similar to that of heart attack.
 |
Given the disease burden of strokes, prevention is an important public health concern. As Stroke Neurosurgeons, we do not want to treat acute stroke, due to much higher risks are involved in emergency settings. However we are forced to do so in order to save lives of patients who are suffering from acute stroke. Actually we want to prevent stroke by promoting stroke risks screening program and stroke prophylactic treatments.
 |
 |
 |
 |
 |
 |
What risk factors for stroke can't be changed?
Age — The chance of having a stroke approximately doubles for each decade of life after age 55. While stroke is common among the elderly, a lot of people under 65 also have strokes. Nowadays due to lifestyle factors, more young adults aged 30-50 years suffered from stroke.
Heredity (family history) — Your stroke risk is greater if a parent, grandparent, sister or brother has had a stroke. The familial trend correlates with that of hypertension, hypercholesterolemia and diabetes mellitus.
Sex (gender) — Stroke is more common in men than in women. In most age groups, more men than women will have a stroke in a given year. However, use of birth control pills and pregnancy pose special risks to female stroke patients, thus more than half of total stroke deaths occur in women. Hence at all ages, more women than men die of stroke.
Prior stroke, TIA or heart attack — The risk of stroke for someone who has already had one is many times that of a person who has not. If you've had a heart attack, you're at higher risk of having a stroke, too.

What stroke risk factors can be changed treated or controlled?
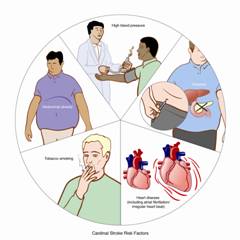
Poor diet — Diets high in saturated fat, trans fat and cholesterol can raise blood cholesterol levels. Diets high in sodium (salt) can contribute to increased blood pressure. Diets with excess calories can contribute to obesity. Also, a diet containing five or more servings of fruits and vegetables per day may reduce the risk of stroke.
Physical inactivity and obesity — Being inactive, obese or both can increase your risk of high blood pressure, high blood cholesterol, diabetes, heart disease and stroke. Try to get a total of at least 30 minutes of activity on most or all days.
Regular resting time & sleep---In our clinical experience, recent illness, inadequate rest and sleeping pattern trigger stroke attack in patients who are already stroke prone by their preexisting risk factors.
Cigarette smoking (active and passive)— In recent years, studies have shown cigarette smoking to be an important risk factor for stroke. The nicotine and carbon monoxide in cigarette smoke damage the cardiovascular system in many ways.
Drugs---The use of oral contraceptives combined with cigarette smoking greatly increases stroke risk. Soft drugs abuse also impose risk of having a stroke.
Alcohol abuse — Alcohol abuse can lead to multiple medical complications, including stroke. Excessive alcohol consumption can cause stroke. For those who consume alcohol, a recommendation of no more than two drinks per day for men and no more than one drink per day for non-pregnant women best reflects the state of the science for alcohol and stroke risk.

High blood pressure — High blood pressure is the leading cause of stroke (accounts for 35-50% of stroke risk) and the most important controllable risk factor for stroke. Many people believe that effective treatment of high blood pressure is a key reason for the accelerated decline in the death rates for stroke. However in some special clinical conditions i.e. in patients with pre-existing of vascular stenosis e.g. Carotid artery stenosis, a slightly higher blood pressure level are needed to be tailored-made by a stroke neurosurgeon.
High blood cholesterol — High blood cholesterol cause atherosclerosis and thus increased the risk for stroke. It appears that low HDL ("good") cholesterol is a risk factor for stroke in men, but more data are needed to verify its effect in women. Lipid lowering drugs have been shown to reduce the risk of stroke by about 15%
Diabetes mellitus — Diabetes carries familial trend and is an independent risk factor for stroke. Diabetes mellitus increases the risk of stroke by 2 to 3 times. Many people with diabetes also have high blood pressure, high blood cholesterol and are overweight. This increases their risk even more.
Carotid or intracranial artery disease — The carotid arteries in your neck supply blood to your brain. Carotid artery stenosis is a disease caused by atherosclerosis fatty deposits forming a plaque to narrow the lumen of the artery. The blood flow to supply brain was thus jeopardized; it may or may not cause symptoms to patient. Sometimes small fatty deposits at arterial wall may dislodge, flow distally and block the brain vessels and cause embolic stroke. Sometimes the disease also made the carotid artery being prone to injury (arterial dissection injury) or prone to be blocked by a blood clot, thus leading to major stroke. When the artery disease happens at arteries inside the brain i.e. intracranial artery stenosis, it will also cause stroke in a similar manner.
Peripheral artery disease — This is the narrowing of blood vessels carrying blood to limbs and organs. It's caused by fatty buildups of plaque in artery walls. People with peripheral artery disease have a higher risk of carotid artery disease or intracranial vessels disease, which raises their risk of stroke.
Atrial fibrillation — Being common in elderly, this heart rhythm disorder raises the risk for stroke. The heart's upper chambers quiver instead of beating effectively, which can let the blood pool and clot. If a clot breaks off, enters the bloodstream and lodges in an artery leading to the brain, a stroke results. Those with atrial fibrillation have a 5% a year risk of stroke, and this risk is higher in those with valvular atrial fibrillation. [Depending on the stroke risk, anticoagulation or anti-platelet drugs is warranted for stroke prevention
Other heart disease — People with some types of congenital heart defects, heart valve disease, coronary heart disease, dilated cardiomyopathy (an enlarged heart), heart failure have a higher risk of stroke than those with hearts that work normally.
Transient ischemic attack (TIA)
Transient ischemic attack (TIA) is "warning stroke", is the strong predictor of a major stroke. It (TIA) is also often known as "minor stroke" that produce stroke-like symptoms but of no lasting brain damage. It is also caused by a mini-clot that cause transient blockage to blood vessels. As the blockage is transient, unlike a major stroke, there is no permanent damage to the brain. Nevertheless, TIA is an important signal of a major stroke. A person who's had one or more TIAs is almost 10 times more likely to have a stroke than someone of the same age and sex who hasn't. And 1/3 of people with TIAs experience a major stroke in the same year. Therefore recognizing and treating TIAs can reduce your risk of suferring a major stroke. TIA should be considered as medical emergency. It is essential to grasp TIA’s symptoms and followed up immediately with a stroke neurosurgeon, and should be treated in the same way as a stroke.