NEUROSURGERY is a highly specialized surgical subspecialty that involves i) medical treatments ii) physical treatments iii) interventional or endovascular procedures and iv) minimally invasive microsurgeries for treating a very wide spectrum of clinical conditions and diseases that happen at our BRAIN and SPINE. Among all, treating STROKE and PAIN are the basics of Neurosurgery daily practices.
In the other words, NEUROSURGEONs, with their knowledges and trainings, together with their sophisticated micro-instruments, utilize their operative skills under the microscope, they treat wide spectrum of clinical conditions and diseases that happen along human nervous systems and its surrounding tissues; skull, spinal column, vessels and related tissues.
The followings are the summary of the common routines in Neurosurgical Practices:
with numbness, pain, weakness at arms or legs, sciatica pain at legs.
with spinal cord or cauda equina nerves compressions, causing pain, numbness, weakness at arms or legs, disturbed gait, disturbed urinary habit and bowel habits, disturbed sexual function.
with back pain, nerves compressions, spinal instability or scoliosis:
Minimally Invasive Spine Fusion Surgery under Microscope:Among all Neurosurgeries, minimally invasive spine surgery (MIS Spine Surgery) are the microsurgeries that Neurosurgeons most commonly perform among their routines.
For all spine surgeries, Neurosurgeons apply their knowledges of nervous system and spinal column, and also their microsurgical skills and techniques, together with their micro-instruments of brain surgeries. Sometimes, Neurosurgeons may also add the technique of Continuous Intra-Operative Neural Monitoring (IOM) to monitor the nerve signal transmission function along brain, spinal cord and nerves during surgery, so as to assure patients’ good neurological outcome in spine surgeries.
With the ever-advancing Medical Technology, seeking a second medical opinion is now the standard practice for all kinds of medical diagnoses. Getting a second medical opinion from another Medical Expert is a decision-support tool for ratification or modification of the medical suggestions from other doctors.
Second medical opinion may have critical impacts on the disease outcome by influencing the followings, namely 5Cs:
Brain tumors can be subdivided into non-cancerous benign tumor and malignant cancerous tumor. If a tumor is originated within brain compartment ......
Tumors can develop in the vertebrae, nerves, and other tissue throughout your spine. Some spine tumors, such as astrocytomas, occur more commonly in children and adolescents......
Given the disease burden of strokes, prevention is an important public health concern. As stroke neurosurgeons, we do not want to treat stroke unless we are forced to do so for acute stroke ......
Brain tumors grow and compress normal brain tissue. Both benign and malignant tumors can cause swelling of the brain and raised intracranial pressure. Headache, dizziness....
This publication on stroke prevention and management highlights the need to reduce the local burden of stroke through the screening of individuals for stroke risk management and through ensuring a prompt and effective treatment response after stroke onset.
Reducing the burden of stroke
Stroke is a leading cause of death worldwide, with an estimated 5.7 million deaths from stroke in 2005, more than 1.4 million of these in China [1]. In Hong Kong, the annual stroke mortality rates are in excess of 3000 [2]. Stroke is also the commonest cause of permanent disability in adults [2]. The death and disability from stroke is expected to increase in Hong Kong as the population rapidly ages in coming decades [2].
Reducing the burden of stroke in Hong Kong, as elsewhere, depends on effective intervention, specifically:
• Promoting public awareness of stroke through stroke screening & public education
• Screening, assessment and intervention for modifiable risk factors for stroke;
• Consistent use of effective medical treatments for primary and secondary prevention of stroke;
• Prophylactic surgical or endovascular treatments for any organic vascular lesions found during stroke screening
• Rapid recognition of stroke in the community; and
• Timely and effective acute stroke management.
These topics, particularly medical and surgical aspects of stroke prevention and acute treatment, are the focus of this article. However, it is recognised that stroke and stroke recovery has a wider impact on families, carers and the community and that multidisciplinary rehabilitation is a key component of care for stroke survivors.
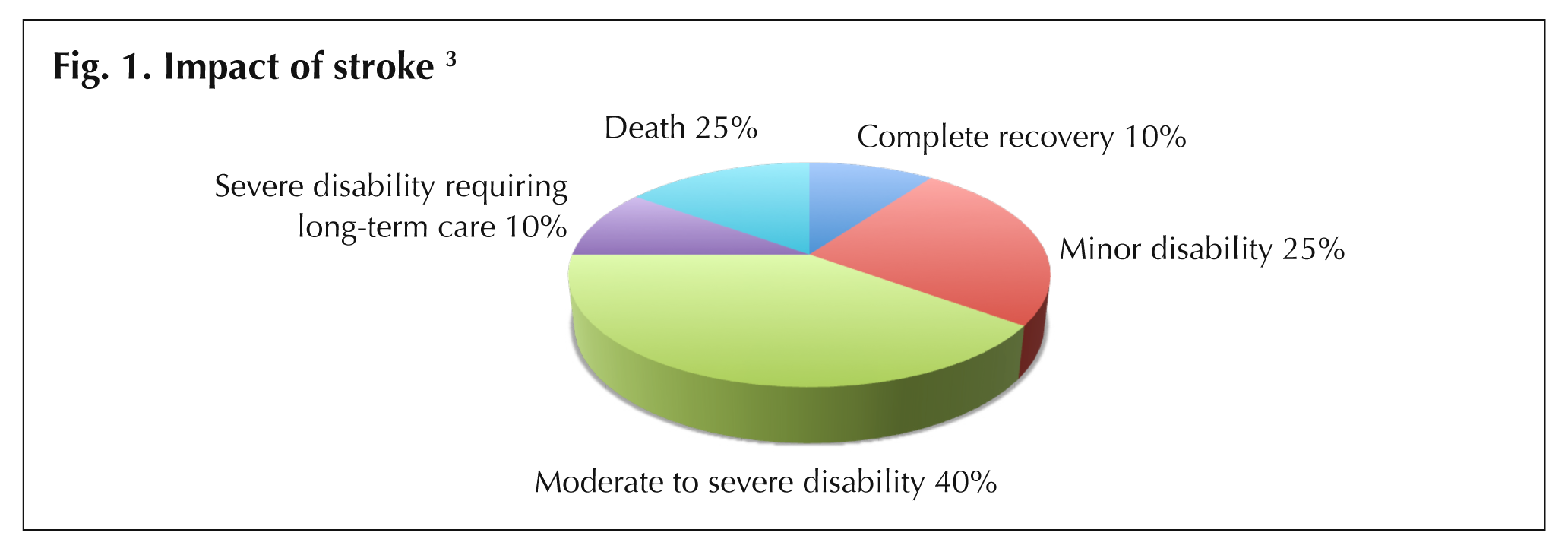
Stroke survivors experience a variety of outcomes that are determined by their age, severity of stroke, and the success and timing of treatment [3]. General stroke recovery rates are shown in Fig. 1 (Impact of stroke).
Improved treatments and more timely treatment have the potential to positively influence these outcomes for both individuals and their families.
 Risk factors for strokeScreening for stroke
Risk factors for strokeScreening for stroke
The majority of strokes are preventable and thus prevention continues to be a key aspect of reducing the burden of stroke for individuals and the wider community [4]. This can be achieved through screening individuals for known risk factors for stroke and implementing management of modifiable risk factors. In the United States, most stroke centres recommend starting stroke screening for adults from 18 years of age.
Recognised risk factors for ischaemic stroke are summarised in Table 1, with modifiable risk factors signifying potential areas for lifestyle, medical or surgical interventions.
| Table 1. Risk Factor for ischaemic stroke [5,6] | |
| Modifiable risk factors | |
| • Obesity | • Other extra or intracranial vascular abnormalities |
| • Smoking | • Coronary heart disease |
| • Alcohol abuse | • History of stroke or TIA |
| • Lack of exercise | • Atrial fibrillation |
| • Hypertension | • Valvular heart diseases |
| • Diabetes mellitus | • Hypercoagulable states |
| • Hypercholesterolaemia | • Homocysteinaemia |
| • Severe carotid stenosis | • Connective tissue diseases |
| • Intracranial arterial stenosis | |
| Not able to be modified | |
| • Increasing age | • Family history |
| • Male sex | • Race / ethnic group |
Insights from the INTERSTROKE study
The recently published findings of the INTERSTROKE study [6] have added a great deal to the understanding of specific risk factors for stroke. This study, conducted in 22 countries worldwide, investigated risk factors for ischaemic and intracerebral haemorrhagic stroke in 3000 cases with 3000 matched controls.
The INTERSTROKE study found that the 10 most significant risk factors for all stroke were: hypertension, current smoking, waist-to-hip ratio, diet risk score, low levels of physical activity, diabetes mellitus, alcohol intake of more than 30 drinks per month or binge drinking, psychosocial stress, depression, and cardiac causes. These risk factors collectively accounted for approximately 90% of the risk of stroke.
In keeping with earlier studies, the INTERSTROKE study found that hypertension is the most important risk factor for all types of stroke and is a more potent risk factor for haemorrhagic than ischaemic strokes. Hypertension was also shown to be a particularly important risk factor in people 45 years or younger.
Screening at the hong kong stroke centre
Screening at the hong kong stroke centre is a comprehensive process. It includes:
• History taking and interviewing patients about their lifestyle, personal health, family history and stroke risk
• Clinical and laboratory screening to assess for risk factors
• Imaging screening of the brain using magnetic resonance imaging, and intracerebral and cervical vessel imaging using magnetic resonance angiography
• Risk factor control interventions appropriate to each individual
- Lifestyle modification (eg, dietary advice & weight management, smoking cessation advice, etc)
- Medical therapy (for blood pressure, cholesterolaemia, glycaemic control in diabetes etc)
• Neurosurgical endovascular management (eg, intracranial or extracranial vascular abnormalities, carotid artery stenosis, etc)
Screening promotes stroke prevention and early intervention at the level of each individual patient. It takes a proactive approach to the identification of risks for stroke, including the identification of vascular abnormalities, stenosis, and existing lesions using diagnostic imaging, and also provides interventions as required. Comprehensive stroke screening at the hong kong stroke centre assists the family physician in the ongoing management of each patient.
 |
|
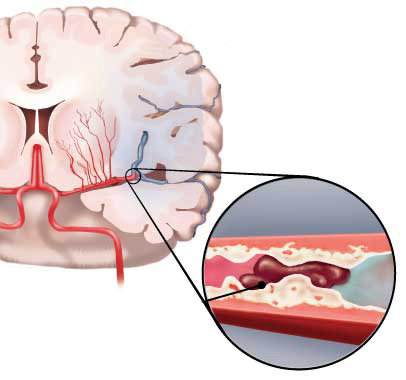
| Fig. 2. Ischaemic stroke: blood clot stops the flow of blood to an area of the brain |
Stroke: New concepts and care
Most strokes are acute ischaemic strokes due to blockage of an artery in the brain (Fig. 2). In Hong Kong, it is estimated that approximately 70% of strokes are ischaemic strokes [5], with the remainder being haemorrhagic strokes. Stroke is a heterogeneous condition and the treatment strategy for these two stroke types differs. It is important that the care of each patient at each phase of intervention is tailored to the individual's needs [5].
The major development in stroke care in the last decade is the recognition that acute ischaemic stroke is a medical emergency and that 'time is brain' (see box feature) [7]. This has coincided with the availability of thrombolytic treatment for ischaemic stroke using intravenous recombinant tissue plasminogen activators (rtPAs). More recently, advances have included Percutaneous Cerebral Intervention (Neuro-PCI). These treatments are available at the hong kong stroke centre, with the aim of minimising stroke disability and improving outcomes for individuals with acute ischaemic stroke.
|
Time is Brain • Emergency evaluation and treatment of acute ischaemic stroke is required. Estimates of brain loss per unit time highlight the time urgency of stroke care. • The most common type of ischaemic strokes are large vessel, supratentorial strokes. These strokes typically have an evolution of between 6 to 18 hours. During stroke evolution, it is estimated that 120 million neurons, 830 billion synapses and 714 km of myelinated fibres are lost each hour (Table 2). • Compared with the normal rate of neuronal loss in aging, the ischaemic brain ages 3.6 years each hour of stroke evolution without treatment.
source: Saver JL. Stroke.2006;37:263-266 |
||||||||||||||||||||||||||||
Community stroke recognition and response
A critical step in improving stroke outcomes is ensuring that there is prompt recognition of stroke and rapid access to appropriate treatment facilities. This is essential to ensure patients receive treatment within the therapeutic window for appropriate treatments [8].
Delays in seeking medical attention after stroke/TIA reflect that the patient and those with them fail to recognise the symptoms of stroke/TIA or to seek emergency medical care [9]. The need for greater public awareness is recognised, particularly for those at increased risk of stroke. Through stroke screening, public awareness can be promoted.
The FAST mnemonic (face, arm speech, time) has been shown to identify almost 90% of cases of acute stroke and TIA, with better performance for ischaemic than haemorrhagic stroke [9]. The FAST mnemonic has been used in public awareness campaigns around the world. See the box feature for further details of the FAST.
|
Recognise stroke symptoms F.A.S.T. You can recognise a stroke using the FAST test FACIAL weakness: Can the person smile? Has their mouth or eye drooped? ARM weakness: Can the person raise both arms? SPEECH problems: Can the person speak clearly and understand what you say? TIME to call for emergency medical help: 24-hour emergency hotline +852 3420 6660 If a person fails any one of these tests, get help immediately by dialling 999 A speedy response can help reduce the damage to a person's brain and improve their chances of a full recovery. A delay in getting help can result in death or long-term disabilities. Don't ignore temporary symptoms If symptoms disappear within 24 hours, the person may have had a transient ischaemic attack (TIA), which is also called a mini-stroke. A TIA is still a medical emergency, because it can lead to a major stroke. This version of the FAST has been adapted for asia medical specialists from a version of the FAST content available at www.shetlandlive.com |
3 Golden hours: Benefits and limitations of intravenous rtPA
Intravenous rtPA is a proven, established treatment for acute ischaemic stroke [10,11] and is recommended in local and international guidelines for acute stroke treatment [4,5,12]. It needs to be delivered in a well-equipped centre with relevant expertise to allow rapid assessment, investigation, treatment & monitoring [12]. Accepted indications for use of this treatment are as presented in Table 3.
The therapeutic benefit of IV rtPA is strongly time dependent and is greatest when given early after stroke onset and declines over 3 to 4.5 hours. Studies have shown that starting this treatment within 90 minutes of stroke onset is optimum and that for every 10 minute delay within the 1-3 hour treatment time period, 1 fewer patient has an improved disability outcome [10]. This has led to initiatives aimed at achieving thrombolysis - so-called 'door to needle' times - of within 60 minutes. The American Heart Association/American Stroke Association is currently promoting a goal of 50% of patients with ischaemic stroke having a door to needle time of ≤60 minutes [13].
Key strategies identified to meet this goal include:
• Emergency medical service pre-notification
• Activating the stroke team with a single call
• Rapid access to and interpretation of brain imaging
• Specific protocols and tools for acute stroke management
• A team-based approach
Symptomatic intracranial bleeding is a recognised and serious side effect of IV rtPA and is estimated to affect approximately 6% of patients [11]. Salvage neurosurgery is a difficult undertaking if intracranial bleeding occurs but is an option in specialist neurosurgical centres, such as the hong kong stroke centre.
| Table 3. Patient Selection Criteria for IV rtPA |
| Indications [12] |
| • Onset of ischaemic stroke within the preceding 3 hours • Measurable and clinically significant deficit on National Institute of Health Stroke Scale (NIHSS) examination • Patient's brain imaging does not show haemorrhage or non-vascular cause of stroke • Patient's age is >18 years |
| Contraindications [14] |
| • Age < 18 • CT scan findings (intracranial haemorrhage, or major acute infarct signs) • Suspicion of subarachnoid haemorrhage (even if head CT is negative for haemorrhage) • Recent (within 3 months) major surgery or trauma (discuss with Attending) • History of intracranial haemorrhage or brain aneurysm or vascular malformation or brain tumor (May consider IV tPA in patients with CNS lesions that have a very low likelihood of haemorrhage, such as small unruptured aneurysms or benign tumors with low vascularity) • Known bleeding diathesis OR 1. Current use of oral anticoagulants with INR > 1.7 or PT > 15 seconds 2. Use of heparin within 48 hours preceding onset of stroke AND prolonged aPTT at time presentation 3. Platelets <100,000 4. Internal haemorrhage (GI haemorrhage, urinary tract haemorrhage) < 3 weeks 5. Dabigatran use in the past 48 hours (if last dose >48 hours, confirm normal renal function [creatinine clearance >50 mL/min] and normal coagulation [aPTT, INR, platelet count] before tPA administration). 6. Low molecular weight heparin use (i.e.- Lovenox) in the past 24 hours. • Persistent systolic BP >185 mm Hg or diastolic BP >110 mm Hg despite treatment. |
8 Golden hours: Neurointerventional techniques for acute ischaemic stroke
Neuro-PCI
• Intra-arterial thrombolysis (ia rtPA)
• Mechanical thrombectomy
• Intravascular stenting
These treatments can be offered in highly specialised centres with advanced imaging and neurosurgical specialisation. They may be used alone or in combination. A major advantage of these treatments is that they are of benefit beyond the period that intravenous rtPA thrombolysis is effective. They extend the therapeutic window for acute ischaemic stroke treatment from 3 hours, offering up to '8 Golden hours'.
Neuro-PCI treatment depends on detailed brain angiography to look for the causative vascular occlusive lesion that PCI will target. The use of neuro-PCI for stroke is similar to the use of cardiac PCI for acute coronary ischaemia. In the United States, comprehensive stroke centres with a vascular neurosurgical service may prefer neuro-PCI over intravenous rtPA treatment because of the reduced risk of bleeding complications. When intra-arterial rtPA is used as part of a neuro-PCI intervention, a very low dose of rtPA is directly infused as an adjunct to mechanical thrombectomy to lyse the blocking thrombus.
Recent data from the MERCI/Multi MERCI trials patients showed that as many as 40% of those who had successful revascularisation with such treatments at 6.9 hours or later after stroke onset still achieved independent functional outcomes [15].
Appropriate treatment should be started as soon as possible after stroke onset for the best outcome. However, in special clinical conditions some patients presenting up to 8 hours after stroke onset, can still benefit from neurointervention.
Mechanical thrombectomy
Brain revascularisation can be achieved by mechanical thrombectomy under the fluoroscopic guidance of cerebral angiograms (Fig. 4). There are a range of clot retrieval devices that can potentially be used for mechanical thrombectomy [16].
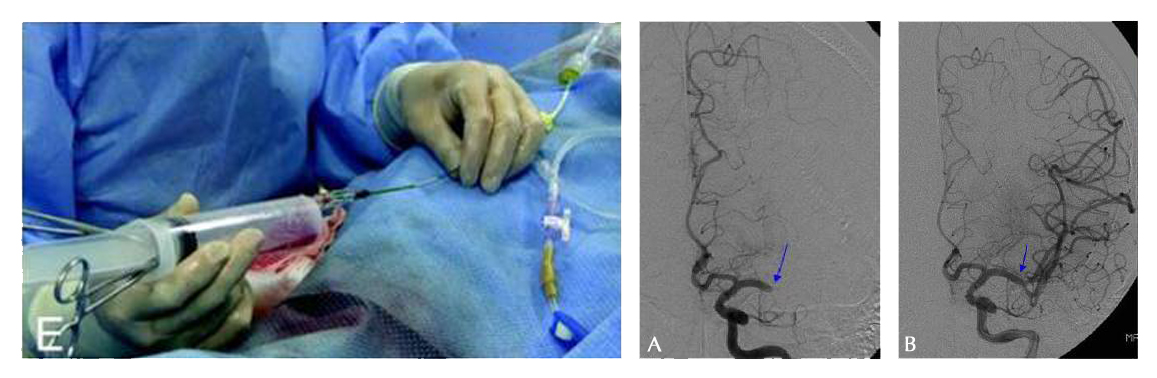 |
| Fig. 4. Mechanical thrombectomy revascularising the brain A - Pretreatment angiography shows total occlusion of the M1 segment of the left middle cerebral artery (MCA) (arrow). B - Immediate post-procedural angiography shows complete revascularisation (arrow). |
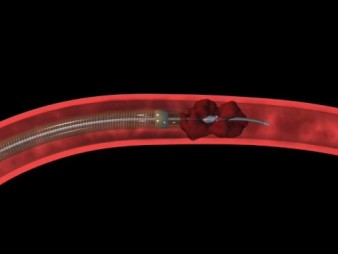
With clot retrieval devices, a guidewire and micro-catheter is passed up to the occluding clot in the intracranial vessel. The thrombus or embolus is then removed by the device using mechanical breakage and aspiration. Clot retrieval devices, such as the MERCI Retrieval System (Concentric Medical Inc., California, USA) (Fig. 5) have been the most well-researched [16] and the MERCI system has now been in use in the USA and Europe for several years [17]. A systematic review of 23 small observational studies found that those treated with clot removal devices were about 15 times more likely to have a good outcome (modified Rankin score ≤2) and 2.2 times less likely to die [16].
The Penumbra System (Penumbra, Alameda, California, USA) [17] is a more recent device also designed for use in acute ischaemic stroke secondary to large vessel thromboembolism (Fig. 6).
 |
 |
| Fig. 5. The Merci Clot retriever for mechanical thrombectomy | Fig. 6. The Penumbra System for mechanical thrombectomy |
Intra-arterial thrombolysis
Injection of IA rtPA at the site of the thromboembolism improves outcomes in acute ischaemic stroke. A Cochrane review found that IA thrombolysis resulted in a significant reduction in the combined odds of death and dependency at follow-up [11].
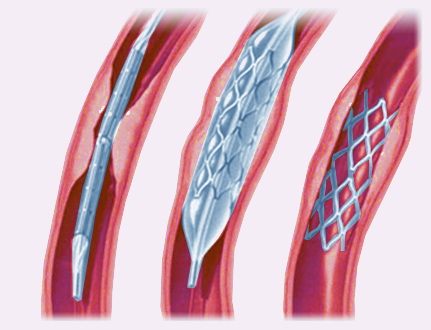
Use of intravascular stents
With advances in endovascular stent design and delivery, stenting has recently become a feasible treatment option for neurovascular disease [18]. Stents initially conceived for treatment of intracranial atherosclerosis (Wingspan stent - Fig. 7) and for aneurysm remodelling (Enterprise and Neuroform stents) have paved the way for new therapeutic approaches in acute ischaemic stroke [19].
 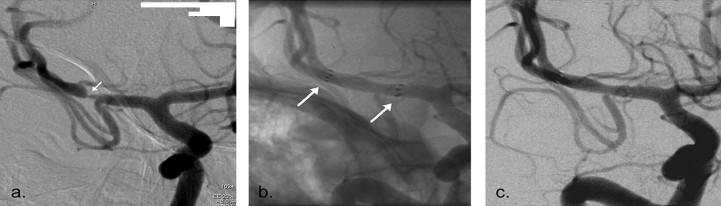 |
| Fig. 7. The Wingspan stent. A - The Pre-stenting angiogram (DSA) showing right MCA stenosis B - stent-in-situ with stent marker (white arrow). C - the post-stenting DSA |
Clinical studies to date have shown that stents are efficacious in the treatment of acute ischaemic stroke [18].
| Potential advantages of neuro-PCI | |
| Neuro-PCI | Intravenous rtPA |
|
Extends the therapeutic window from 3 hours up to 8 hours. Neuro-PCI offers a treatment option for those with acute stroke who do not access specialist medical services within 3 hours. Effective neuro-PCI revascularisation in the 4th to 7th hour may salvage brain cells in the Penumbra Zone (peripheral ischaemic region) minimising the area of infarction. |
Accepted therapeutic window for treatment is 3 hours. Studies show optimum use is within 90 minutes [10]. These time-to-treatment intervals have proved generally difficult to achieve due to patient factors, lack of community awareness and access and provision of appropriate medical services. |
|
Neuro-PCI may be suitable for individual patients who: a) have a contraindication to intravenous rtPA; or b) have not had an adequate therapeutic response to intravenous rtPA. |
Symptomatic intracranial bleeding is a recognised and serious side effect of IV rtPA and is estimated to affect approximately 6% of patients [11]. |
| Intra-arterial delivery of lytic agents may increase the chance of recanalisation. | Occlusions in some areas (e.g. proximal middle cerebral artery) are known to be more resistant to intravenous delivery of lytic agents [20]. |
Summary
Stroke is a brain attack and time is brain.
Prevention through screening and risk factor control is the best possible treatment.
Awareness of stroke symptoms and rapid access to emergency medical care is necessary to improve outcomes.
Neurointervention techniques now allow effective acute ischaemic stroke treatment for up to a GOLDEN 8 HOURS.
References
|
Dr Yiu Ting Kan MBBS (HK), FRCS (Edin) Brain and Spine Neurosurgery Languages Spoken:English, Cantonese |
 |
Brain Tumours:
Tumour excision - minimally invasive surgery by neuronavigation, microscopy and endoscopy; awake craniotomy/fluorescence-guided glioma excision for function-preservation
Endoscopic Endonasal Transsphenoidal Surgery
Vascular:
Functional Neurosurgery:
Paediatric Neurosurgery:
Radiosurgery:
Spine:
Trauma Surgery:
Peripheral Nerves:
A stroke is a serious medical condition that occurs when the blood supply to part of the brain is cut off. Strokes are a medical emergency and prompt treatment is essential - the sooner a person receives treatment for a stroke, the less damage is likely to happen.
Our 24 hours stroke care hotline, our neurosurgeon to optimize every patient's specific diagnosis and provide high quality standards of care. We have strong links with private hospital in Hong Kong, Kowloon and New Territories.
中風有時也會被稱為腦血管意外(Cerebrovascular Accident CVA), 是影響頸部血管或大腦血管的一種疾病,從而干擾到大腦的供血或腦壓, 迅速領到大腦功能喪失。
為什麼腦中風的危險因素不能改變?
年齡 — 在55歲以後生活的每個十年有腦中風的機率大約增加一倍,。雖然腦中風是老年人中常見,很多65歲以下的人也中招。現在,由於生活方式的因素,年齡在30-50歲的成年人也受到影響。
遺傳(家族史) — 如果父母,祖父母,兄弟姐妹曾有腦中風的經驗, 你腦中風的風險是更大的。家族性趨勢水平通常與高血壓,高膽固醇血症和糖尿病有關。
性別 — 患腦中風是多見於男性多於女性。在多數年齡組,男性多於女性。然而,使用避孕藥和懷孕帶來的特殊風險,以女性腦中風患者,從而超過總數
中風前或心臟病發作 — 腦中風的人已經有很多次中風,一個人誰沒有的。如果你有一個心臟病發作,你腦中風的風險較太。
為什麼腦中風的危險因素是可以改變的治療或控制?
不良的飲食習慣 — 飲食高飽和脂肪,反式脂肪和膽固醇能提高血液中的膽固醇水平。飲食高鈉(鹽)可以促進血壓升高。常餐中添加多餘的熱量可導致肥胖。此外,包含五個或更多份水果,每天蔬菜的飲食可以降低腦中風的風險。
缺乏體力活動和肥胖 — 作為不活動,肥胖或兩者都可以增加你的高血壓,高血脂,糖尿病,心臟疾病和腦中風的風險。每天試圖得到一個總活動對大多數至少30分鐘。
定期休息時間和睡眠 — 在我們的臨床經驗,最近生病,休息不足,患者比較容易腦中風,睡眠模式觸發腦中風發作的風險也存在。
吸煙 (主動和被動) -近年來,有研究表明,吸煙是腦中風的重要危險因素。香煙煙霧中的尼古丁和一氧化碳在許多方面損害心血管系統。
藥物 — 使用口服避孕藥加上吸煙會大大增加腦中風的風險。濫用軟性毒品亦存在腦中風的風險。
濫用酒精 — 酗酒可導致多種並發症,包括腦中風。過量飲酒可引起腦中風。對於那些喝酒每天不超過兩杯的人士,男性的建議每天不超過一杯,非懷孕婦女最能反映科學酒精和腦中風風險的狀態。
高血壓 — 高血壓是腦中風的主要原因(佔腦中風風險的35-50%)和腦中風的最重要的可控危險因素。許多人認為,有效的治療高血壓是一個關鍵因為它可令腦中風死亡率的加速下滑。然而,由腦中風神經外科醫生一些特殊的臨床情況發現患者與預先存在的血管狹窄如頸內動脈狹窄,需要稍高的血壓水平進行調整,。
高血脂 — 高血脂引起動脈粥樣硬化,從而增加腦中風風險 。看來,低高密度脂蛋白("好"膽固醇)對腦中風的男人是一個危險因素,但需要更多的數據來驗證的婦女其效果。降脂藥物已經顯示了約15%,能減少腦中風的風險
糖尿病 — 進行家族病調查,糖尿病是腦中風的獨立危險因素。糖尿病增加腦中風的風險至3倍。許多糖尿病患者也有高血壓,高血脂和超重。這更增加了他們的風險。
頸動脈或顱內動脈 — 在你的脖子供應血液到大腦的頸動脈- 。頸動脈狹窄是引起動脈粥樣硬化的脂肪沉積形成斑塊縮小動脈管腔的疾病。因此,血流供應大腦受到損害,它可能會或可能不會引起症狀患者。有時小的脂肪沉積在動脈壁會移動,遠端流動和阻止腦血管,造成栓塞性腦中風。有時本病也取得了頸動脈是容易受傷(動脈夾層傷),或容易被阻塞血塊,從而導致嚴重腦中風。當動脈病發生在腦即顱內動脈狹窄的動脈內,這也將導致腦中風的類似方法。
外週動脈疾病 — 這是運載血肢體和器官的血管狹窄。它在動脈壁造成斑塊的脂肪建立。患有外週動脈疾病有頸動脈疾病或顱內血管性疾病,這引起了腦中風的風險較高。
心房顫動 — 作為常見於老年人,這種心臟節律紊亂引起的腦中風風險。心臟的上腔顫動,而不是有效地跳動,它可以供應血池和血塊。如果血塊脫落,進入在動脈導致腦,導致腦中風的血液和心房。那些與心房顫動每年有5%的腦中風風險,而這種風險是高於那些與瓣膜性房顫。[根據腦中風的風險,抗凝或抗血小板藥物是必要的腦中風預防
其他心臟疾病 — 人與某些類型的先天性心臟缺陷,心臟瓣膜病,冠狀動脈心臟疾病,擴張型心肌病(心臟擴大),心臟衰竭患有腦中風的人比那些心臟中正常的人風險較高。
中風是因為腦部動脈血管出現問題而起,三十歲後中風的發病率會以倍數增加。其實,中風的病變是有跡可尋的,透過中風風險評估,我們可清楚了解腦部血管的健康狀況,及早處理問題,減低中風風險。
香港大約有七成的中風個案屬於急性缺血性中風。症狀雖然沒有像出血性中風的來得突然`嚴重和迅急, 但缺血性中風的急性治療卻要比出血性中風治療需求更加快和緊急,因為如果可以在黃金八小時內迅速打通血栓塞的腦血管,缺血的腦細胞就可以重新獲得血液供養, 大腦細胞受損的程度可減至最輕, 病人獲得治愈及完全康復的機會就可大大提升, 有些病人甚至可以完全沒有中風的後遺症和傷殘。
傳統黃金3至4.5小時治療方案的不足
治療急性缺血性中風 (AIS)的傳統方案,是於中風症狀出現後的三至四個半小時內於靜脈注入溶血劑(組織胞漿素原活化劑/recombinant tissue plasminogen activator) (iv rtPA),亦即Activase。但病人往往因為送院太遲、或因診斷的延誤、 或因被歸類為不宜使用溶血劑,所以超過九成半的急性缺血性中風病人, 都不能從黃金3至4.5小時靜脈注入溶血劑的治療方案獲益。
此外,靜脈注入溶血劑rtPA的黃金3至4.5小時治療方案可能無法有效地 治療某類型的缺血性中風: 如中風是因為大血管閉塞, 或是因為過長血凝塊阻塞, 或是因為閉塞性動脈夾層, 或是因為血管創傷而引起的缺血性中風,靜脈注入溶血劑rtPA都可能無效。
大腦通波仔,治療急性中風的黃金八小時
香港腦脊中風及痛症顧問中心 推出治療急性缺血性中風的嶄新「黃金八小時」概念: 腦內血管介入的微創手術(機械式吸取血栓術),正正填補了靜脈注入溶血劑rtPA的黃金3至4.5小時治療方案的不足。 病人可於中風症狀出現後的八小時內接受腦內血管介入的微創手術(機械式吸取血栓術),把血管再次灌通。就像心臟的通波仔微創手術, 專攻腦內血管治療的神經外科醫生會從腹股溝把微型導管放入腦血管,擊碎及吸走腦內血栓,把血管再次灌通, 令腦細胞重獲生機。腦內血管微創手術在大腦血管造影導引下,不但能於大腦栓塞的確實位置進行治療,高度準確地移除血栓。 有時候,如果神經外科醫生發港現病變和狹窄的腦動脈, 而其是造成中風的主要原因,醫生植入柔軟的金屬支架, 將大腦動脈重建。
鑑於中風的疾病負擔甚高,預防中風是一個重要的公共衛生議題。作為專門治療中風的腦神經外科醫生,我們並不想治療急性中風,因為治療急性中風的風險甚高, 但在緊急情況下, 為着拯救生命, 我們都被迫為之。但其實我們是希望提倡防止中風,促進中風風險篩查及中風預防性治療。
中風倖存者容易在未來再中風?
是 - 曾中風的人比正常健康的人有更高的再次中風個風險。如果你曾有心臟病發的病史,你再次中風個風險也是高較。
治療中風的真正成因,以防止短時間內再次中風:
採用傳统的醫療方法,大多數中風治療是盲目性的,無需檢索中風的真正原因而盲目下藥。現時專門治療中風的腦神經外科醫生則會以高品質的MRI造影或腦血管造影,以檢索中風的真正成因, 並把相應的中風風險移除,從而防止中風在短時間內再次發生。
中風患者能否成功地完全恢復健康,物理治療師是一個十分重要的角色。物理治療對中風的早期急救及之後的康復訓練十分重要, 即使嚴重中風令病人重度殘障或意識不清,物理治療亦應在中風後立即開始進行,以把握康復的黃金時機及減低中風的可致命併發症-----肺炎、深層靜脈血栓塞及褥瘡等等。
物理治療可以維持病人氣管及肺部的分泌物暢順排出,以減低罹患致命肺炎的風險。中風後,患者癱軟無力的肌肉在接下來的十數天會逐漸呈現繃緊的狀態,即是肌張力過高。如中風患者無法下床行動,小腿肌肉下就大有可能產生可致命的深層靜脈血栓塞(Deep Vein Thrombosis DVT) 的併發症。因此要預防DVT,就要替中風患者穿上具彈性的壓力袜子及定時進行大小腿肌肉按摩; 有時一些罹患DVT的高危病人, 更有可能需要服用抗凝血藥物,以減低患上致命DVT的風險。
在物理治療專注於矯正四肢和身體動作的同時,職業治療的大部份心思就放在協助患者重獲有用及實際的機能上,就以患者需要使用刀叉來吃肉為例,職業治療的主要目的,就是幫助中風患者盡量擴展他們的能力,使他們可以操作一般日常生活的工作,不但可以增强患者的獨立自主,也同時提升了他們的生活品質。
當中風患者情況隱定,職業治療師便會開始評估中風對患者所造成的損傷程度,並列出足以反映患者需要優先考量的狀況,以訂立其需要的治療計劃。
每個患者的期望,或其自主程度都不一樣,治療計劃也有很大的差異。例如,大部份上年紀的老人會希望恢復到可以獨立完成每天的日常瑣事便足夠,但年紀輕的患者也許就希望儘量重獲自己過去的許多技能。
大部份的中風患者都得參與特別的治療活動和工作,這些活動和工作能協助他們重新學習像如廁、梳洗、進食以及穿衣等必需的動作。這些活動和工作都有專門設計過的輔助器,以協肋進行上述的工作;例如,有一種特殊設計的淺平器具,它可以讓切割食物,以及把食物從盤子移到嘴裡等動作變得較容易。職業治療也會試着讓患者參與各種的嗜好和消遣活動,將情緒和心理上的壓力得以緩和,並讓患者覺得自己對家庭和社會仍有貢獻。
當疑似中風患者被送往公立醫院救治時,當值醫生會按病人情況而安排腦部的電腦斷層掃描(CT SCAN) 。CT是一個較經濟的初步影像檢查,但CT只能分辦出患者是屬於出血性中風 (佔30%的中風案例),不能詳细確診患者是否患上腦血管梗塞性中風(佔中風案例大多數的70%)。 CT 在腦血管梗塞性中風發生的首24小時內, 影像是可以完全正常的, 在醫生亦不能確診下, 病人就因此枉枉錯失了在黄金8小時內打通腦血管, 搶救大腦細胞及完全康復的機會。然而兩種中風: 出血性和腦血管梗塞性中風的治療迫切性及方針是截然不同的。
腦梗塞性中風就是大腦或頸血管受阻塞,血液無法流通,令腦細胞功能暫時受影響, 若時間拖延了, 大腦細胞就會死亡, 神經功能亦永久受損。