NEUROSURGERY is a highly specialized surgical subspecialty that involves i) medical treatments ii) physical treatments iii) interventional or endovascular procedures and iv) minimally invasive microsurgeries for treating a very wide spectrum of clinical conditions and diseases that happen at our BRAIN and SPINE. Among all, treating STROKE and PAIN are the basics of Neurosurgery daily practices.
In the other words, NEUROSURGEONs, with their knowledges and trainings, together with their sophisticated micro-instruments, utilize their operative skills under the microscope, they treat wide spectrum of clinical conditions and diseases that happen along human nervous systems and its surrounding tissues; skull, spinal column, vessels and related tissues.
The followings are the summary of the common routines in Neurosurgical Practices:
with numbness, pain, weakness at arms or legs, sciatica pain at legs.
with spinal cord or cauda equina nerves compressions, causing pain, numbness, weakness at arms or legs, disturbed gait, disturbed urinary habit and bowel habits, disturbed sexual function.
with back pain, nerves compressions, spinal instability or scoliosis:
Minimally Invasive Spine Fusion Surgery under Microscope:Among all Neurosurgeries, minimally invasive spine surgery (MIS Spine Surgery) are the microsurgeries that Neurosurgeons most commonly perform among their routines.
For all spine surgeries, Neurosurgeons apply their knowledges of nervous system and spinal column, and also their microsurgical skills and techniques, together with their micro-instruments of brain surgeries. Sometimes, Neurosurgeons may also add the technique of Continuous Intra-Operative Neural Monitoring (IOM) to monitor the nerve signal transmission function along brain, spinal cord and nerves during surgery, so as to assure patients’ good neurological outcome in spine surgeries.
With the ever-advancing Medical Technology, seeking a second medical opinion is now the standard practice for all kinds of medical diagnoses. Getting a second medical opinion from another Medical Expert is a decision-support tool for ratification or modification of the medical suggestions from other doctors.
Second medical opinion may have critical impacts on the disease outcome by influencing the followings, namely 5Cs:
Brain tumors can be subdivided into non-cancerous benign tumor and malignant cancerous tumor. If a tumor is originated within brain compartment ......
Tumors can develop in the vertebrae, nerves, and other tissue throughout your spine. Some spine tumors, such as astrocytomas, occur more commonly in children and adolescents......
Given the disease burden of strokes, prevention is an important public health concern. As stroke neurosurgeons, we do not want to treat stroke unless we are forced to do so for acute stroke ......
Brain tumors grow and compress normal brain tissue. Both benign and malignant tumors can cause swelling of the brain and raised intracranial pressure. Headache, dizziness....
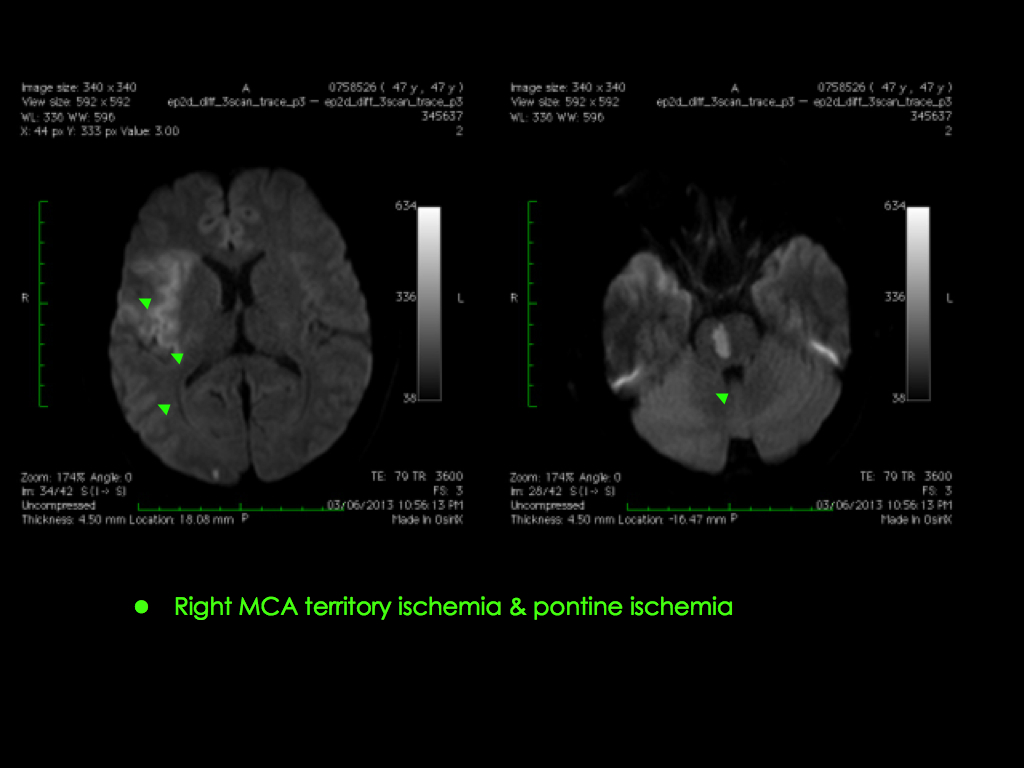
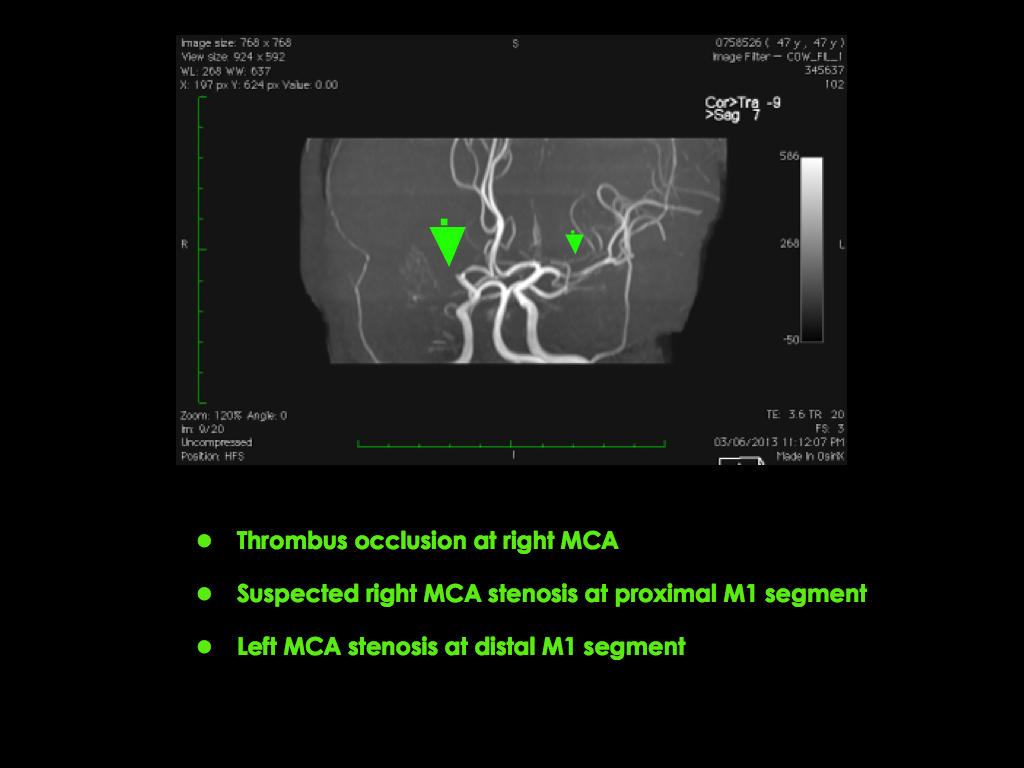
Illustration the new stroke concept with treatment of Neuro-PCI. In 2006, 56 Yrs old Taxi Driver with good past health

Mild dizziness nurse for help, still can walk to toilet on his own. Sudden left limbs severe weakness .....
Symptoms (sudden left limbs flaccid graded 1/5, dysphasia) onset at 19:30, Admitted to public hopsital with plain CT brain reported to be normal. NO active treatment was offered...
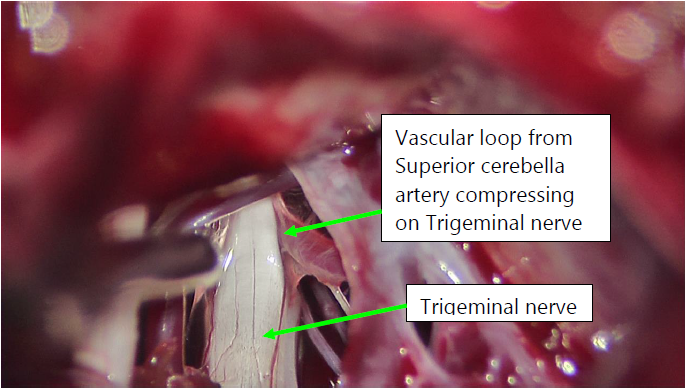
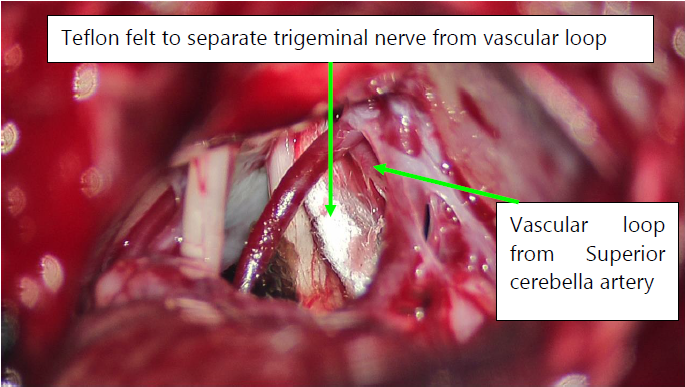
Initial stage of treatment is drug therapy for one or two months. The effectiveness of drugs in controlling the pain can help clinical diagnosis.
But medications can only be a temporary solution, not a permanent cure for the true cause of trigeminal neuralgia that is: external factors compressing on the nerve and make it short-circuit.
Generally doctor will consider medications for
Commonly used drugs include:
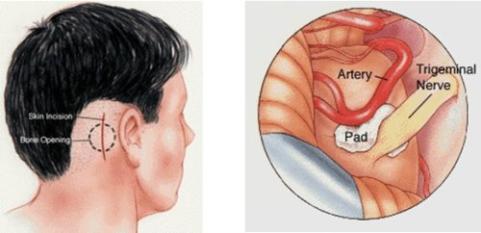
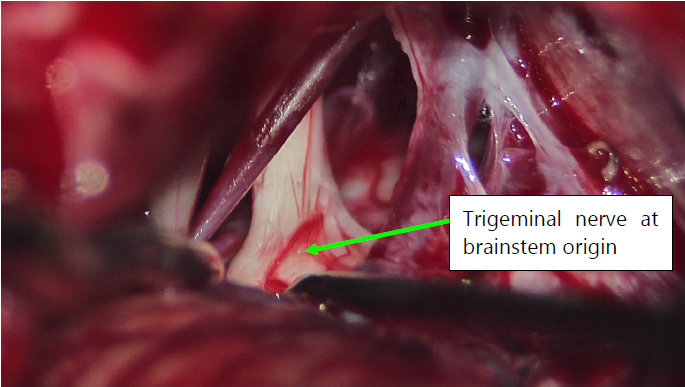
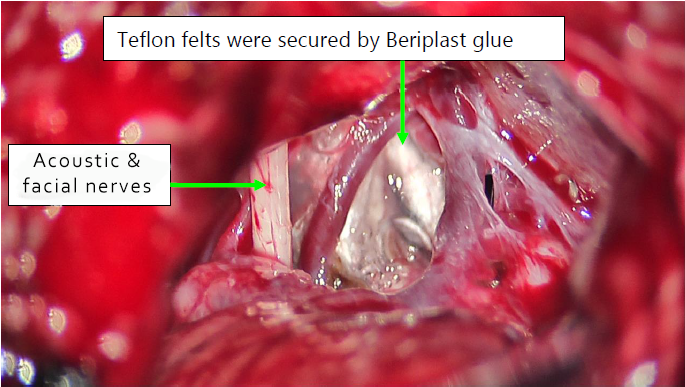
Microvascular decompression of trigeminal nerve:
If delaying treatment, what would be the consequences?
How to determine if they are suffering from trigeminal neuralgia?
Before any invasive procedure or surgery, you should seek professional advice:
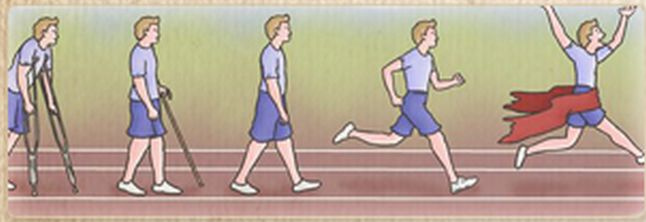
When stroke occurs, brain cells are damaged excessively and some of our brain function is lost.

|
Stroke Rehabilitation should begin as soon as the patient's medical condition has been stabilized. The first aim is to prevent such secondary problems as stiff joints, falls, bedsores and pneumonia. Stroke patients may suffer from disabilities in different areas depending on the part of the brain affected and the severity. |
The first six months after stroke is the Golden-Months for greatest neurological recovery and improvement. From six months onward, recovery progress will begin to slow down over the other 18 months. Therefore it is crucial to grasp the first six months of Golden Rehabilitation Period. Significant neurological improvement at limbs power, awareness and consciousness are expected in most patients if adequate clinical care are provided.

The goal of stroke rehabilitation is to help patients reacquire the ability to carry out the basic activities of daily living, so that they can achieve maximum functionality and independence. After rehabilitation, patients are expected to return to an active and productive lifestyle.
Even though stroke rehabilitation cannot reverse the brain damage, a carefully directed, systematic rehabilitation programme can substantially help patients to reach their maximum potential to live normal lives.
HKBSSP provides quality stroke care and assists patients and their relatives with rehabilitation arrangements. Stroke Rehabilitation team involves doctors, nurses, physical therapists, occupational therapists and speech therapists. Depending on the situation of the patient, individualised programmes are set up specifically suited to the patient's needs in order to regain body functions, mobility, memory, cognitive function, communication skills, and self-care ability.
Rehabilitation can also be arranged to take place at hospitals, sanatorium or home if needed. Depend on individual's need, Traditional Chinese Medicine i.e. acupuncture, Chinese massage, herbal medicine will be part of the rehabilitation programmes.

Physiotherapist plays a very important role in achieving the success of stroke rehabilitation and recovery. Physiotherapy is very important in acute stroke care as well as in stroke rehabilitation. In order to maximize the chance of stroke recovery as well as to reduce lethal stroke related complications e.g. pneumonia, deep vein thrombosis and decubitus ulcers etc, physiotherapy should be started immediately after a stroke; even for patients suffering from severe stroke with gross disability or remaining unconscious

Physiotherapy helps in assisting drainage of bronchial secretion and thus minimize sputum retention, so as to preventing lethal pneumonia. Weeks after a stroke, the muscle tone of the paralysed limbs may be building up to form spastic muscle. Immobilized stroke patients are thus have high risk of developing deep venous thrombosis (DVT) as lethal stroke complication. Pressure stockings and regular muscle massage or limbs stretching help in preventing DVT. For some high-risk patients, oral anti-coagulant drug may be required for DVT prophylaxis.
In order to treat muscle spasticity and to prevent permanent joint stiffness, physiotherapist may regularly stretch the limbs of stroke patients within their normal joints ranges. Physiotherapist will also assess the stroke patient according to the severity of stroke, the affected parts of the body, the lifestyle patterns of the patients and the progress of the initial stroke rehabilitation. Targets and goals of the stroke rehabilitation will then be set. To allow patients for easy practicing and to skill every movement, walking motions are broken down into a few simple actions, stroke patients may relearn walking as a child does.
Stroke physiotherapy starts at bedside, begins with pulling the paralysed muscle and passively stretching the paralysed limbs. This helps to reduce muscle spasticity and joints stiffness. Later on, physiotherapist will guide the patients for body balancing during sitting up and standing up, and teach them how to move back and forth between bed and chair. The next step will be teaching patient how to stand, how to use aids, how to shift their weight from one leg to the other leg. Once physical therapy rehabilitation program begun, intensive treatment schedule will follow. During the initial stages, patients may feel difficult, frustrated, tired and fatigue; however, these movements are essential for long-term stroke rehabilitation. Thus supports and encouragements from medical staffs, relatives and friends are very important to the disabling stroke survivors. Besides, adequate rest and good quality of sleeping at night is also crucial for brain cells recovery.
At last, stroke rehabilitation physiotherapy will not end after hospital discharge. On the contrary, patients should regularly attend physical therapy at hospital, clinic or home for ongoing stroke rehabilitation in order to achieve a sustainable and complete recovery of their impaired neurological functions.
As many as 7 out of 10 stroke patients in Hong Kong have the blockage of the ischaemic type. Although it is less severe than a haemorrhagic one, it calls for immediate treatment to prevent the condition from worsening. That is why we, at the HKBSSP emergency stroke care clinic, are available round-the-clock to help patients in need.

With your complete recovery as our priority, we’ve managed to enhance the efficiency of all our facilities – from logistics to diagnosing and rehabilitation. Following clear-cut protocol guidelines, our neurosurgeons, nurses and other staff work hand in hand so that patients receive high-quality emergency treatment for stroke. As there’s no time to lose, we vouch for timely transfer, brain imaging, diagnosis and on-the-spot care at our centre.
It's of paramount importance to resist the ischaemic attack within the first 8 hours to put brain damage to a bare minimum. This way, we can ramp up your chances of living a healthy and happy life thereafter.
All stroke treatments are time-dependent. How long it takes you to arrive at a hospital after your symptoms start determines the further course of action:
Endovascular Mechanical Thrombectomy for Brain Revascularization.
|
1. The micro-catheter device passed through the vessels |
2. The device breaks the blood clot |
|
|
|
|
|
|
|
||
|
3. The device sucks up the blood clot |
|
4. Blood flow is restored |
|
|
|
|
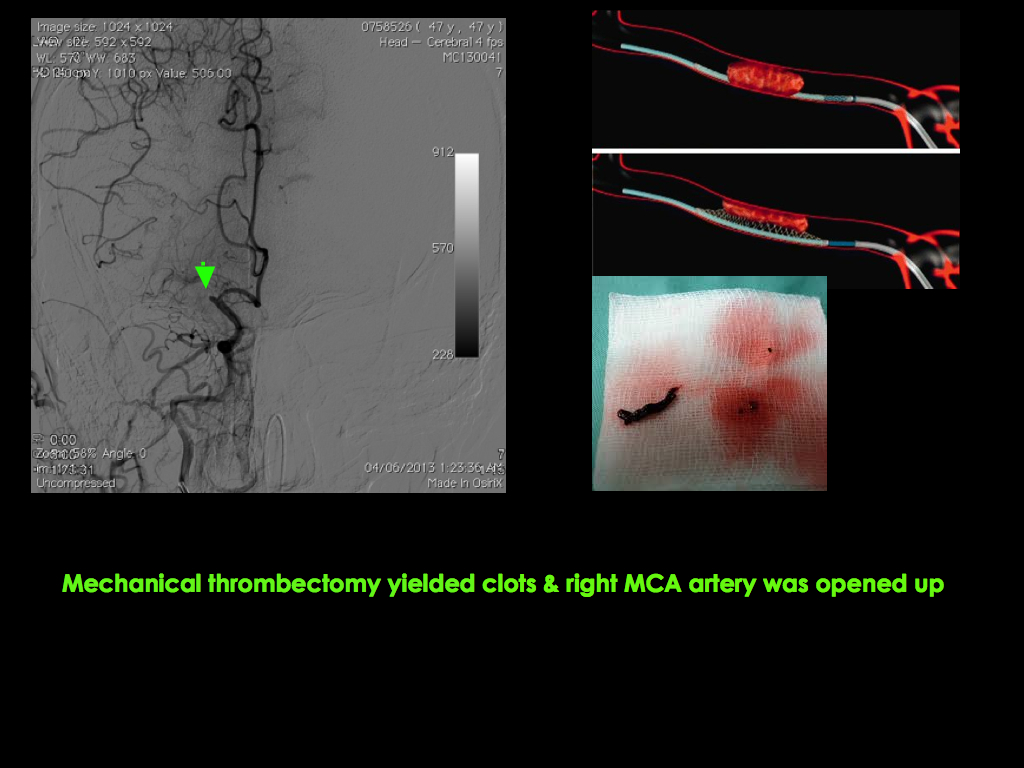
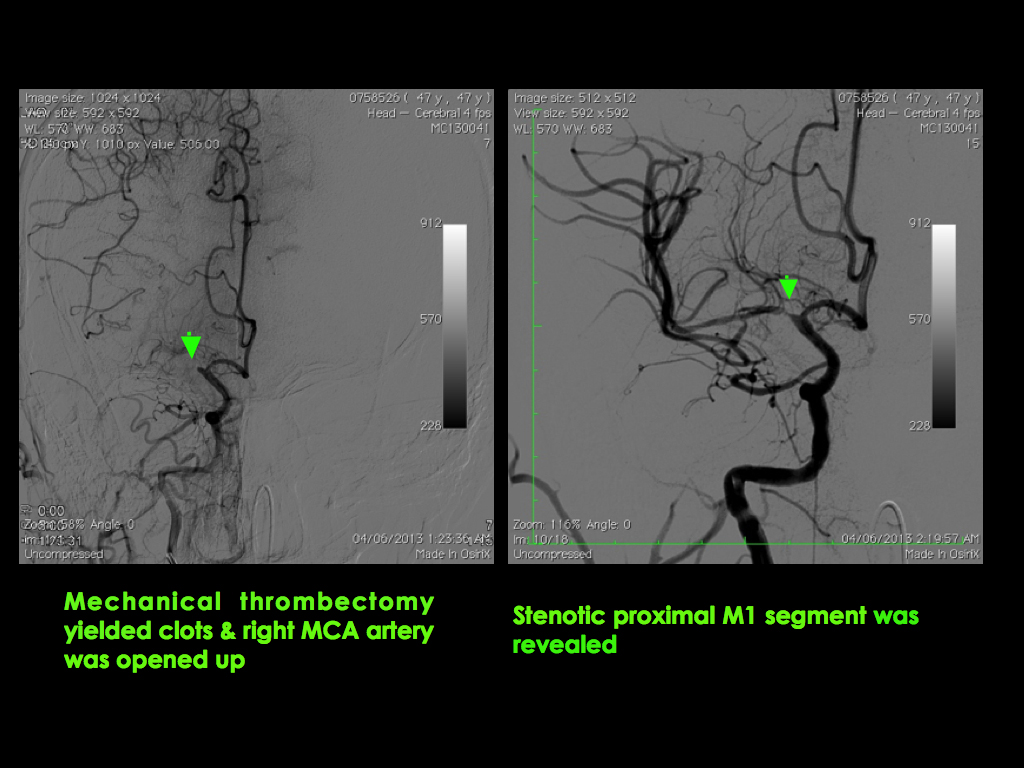
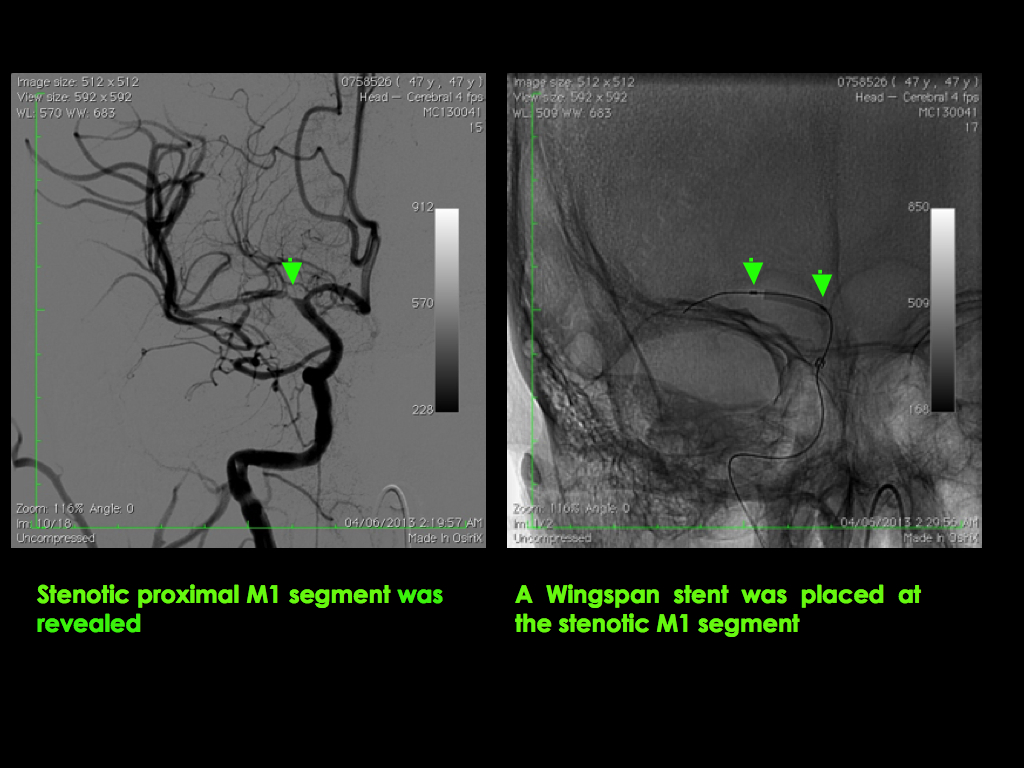
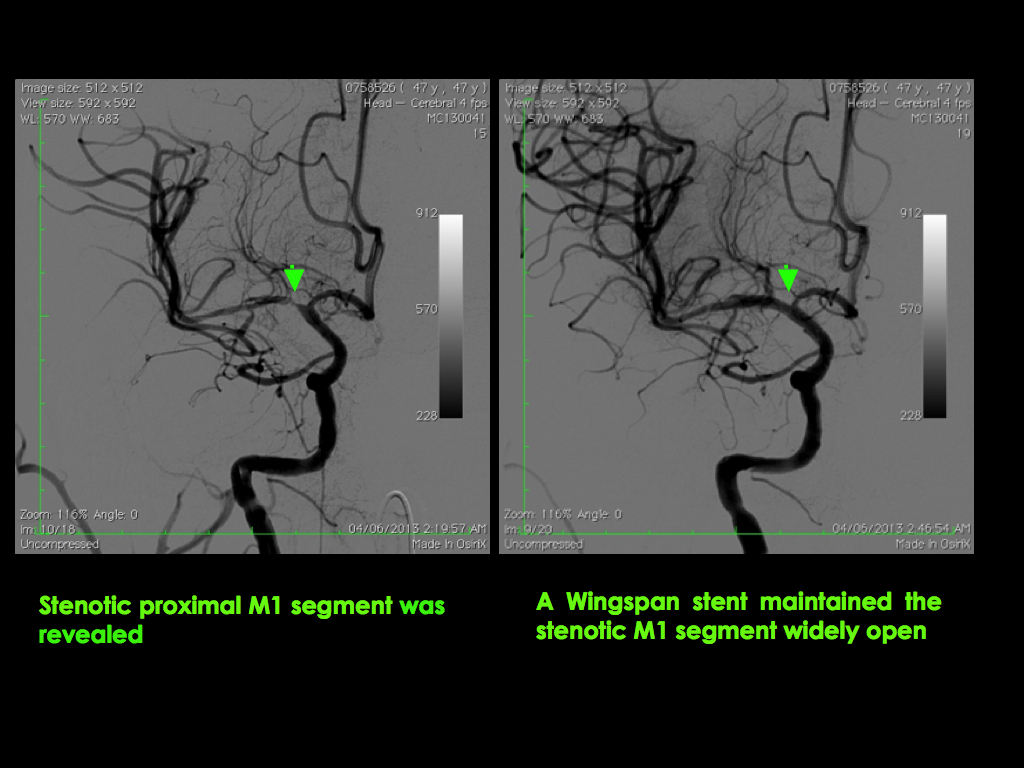
Mechanical thrombectomy is all about unparalleled effectiveness in minimising the effects of acute ischaemic stroke. Plus, some patients may qualify for it even if they show up in 24 hours.
With HKBSSP, your stroke will never be the end of the world!